By Netan Choudhry, M.D, FRCSC and Jennifer George
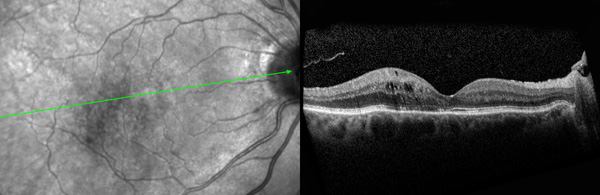
 Optical coherence tomography (OCT) is among the newest non-invasive imaging technologies to surface in modern medicine. Though useful across the medical spectrum, OCT has made its most significant clinical impact in ophthalmology. By measuring reflected light from discontinuities in tissue, OCT applies the principles of interferometry to create three-dimensional cross-sectional images of the retina and anterior segment of the eye with ultra-high spatial resolution. Achieving image resolutions significantly greater than traditional ultrasound technology, OCT images measure between one and 15 microns. Imaging can be performed both in situ and in real time, enabling a wide range of research, clinical and biomedical applications. From start to finish, OCT only takes about five to 10 minutes. An effective, patient-friendly imaging technology, OCT has already been proven to outperform its imaging predecessors.
Optical coherence tomography (OCT) is among the newest non-invasive imaging technologies to surface in modern medicine. Though useful across the medical spectrum, OCT has made its most significant clinical impact in ophthalmology. By measuring reflected light from discontinuities in tissue, OCT applies the principles of interferometry to create three-dimensional cross-sectional images of the retina and anterior segment of the eye with ultra-high spatial resolution. Achieving image resolutions significantly greater than traditional ultrasound technology, OCT images measure between one and 15 microns. Imaging can be performed both in situ and in real time, enabling a wide range of research, clinical and biomedical applications. From start to finish, OCT only takes about five to 10 minutes. An effective, patient-friendly imaging technology, OCT has already been proven to outperform its imaging predecessors.
OCT was the result of collaborative efforts by Tufts University School of Medicine, the New England Eye Center, the Department of Electrical Engineering and Computer Science at MIT, and Lincoln Laboratory at MIT. First demonstrated in 1993, OCT was able to produce in vivo tomographs of the human macula and optic disk. A non-contact imaging technology, OCT provides images of the cornea and angle of the eye in addition to other morphologic aspects of the retina. OCT is much like a vertical biopsy of the retina; however, light is used in place of a knife. Avoiding any physical contact with the eye, OCT of the retina is the most advanced diagnostic tool for diseases of the retina since the emergence of fluorescein angiography.
The images produced by OCT possess such high resolution because the imaging technique is based on light rather than radio frequency or sound. When an optical beam is directed at a tissue, a very small portion of the light reflecting from the tissue is collected. Most of the light is scattered and, rather than forming a clear image, it creates glare. Optical coherence is the principle of physics that allows the filtering of scattered light. During OCT, an interferometer is used to detect only coherent (non-scattered) light. The interferometer removes scattered light from the light that is reflected in order to generate an image that is not only glare-free, but three-dimensional and ultra-high in resolution.
The latest advances in research now allow OCT to possess numerous biomedical applications. It can provide high-resolution images of pathology that would otherwise be challenging to obtain without compromising the physical integrity of the retina. OCT could also prove useful where other imaging technologies yield a high false negative rate, or in the guidance of surgical interventional procedures. OCT has proven to be a useful clinical tool in the imaging of certain macular diseases, including macular edema, macular holes, epiretinal membranes, schisis cavities associated with optic disc pits, macular degeneration, central serous chorioretinopathy and more.
OCT technology in ophthalmology is already into its third generation of devices. The initial devices were based in time-domain technology and, in the second generation of instrumentation, spectral-domain technology was utilized. The resolution increase from time-domain to spectral-domain was a leap forward, allowing for re-characterization of retinal pathologies and providing a deeper understanding of the etiology and natural history of retinal disease such as diabetic edema (Figure 1).
OCT has also enabled eyecare providers to monitor the response of diseases like diabetic retinopathy to treatments such as laser and intravitreal medical therapy, and has thereby become a great teaching tool for patients about their disease state.
The next generation of OCT devices is moving even deeper, towards the most posterior region of the eye. Swept source OCT offers higher resolution at 100,000 A-scans per second and utilizes longer wavelengths of light (1050-nm) to image the eye, offering simultaneous anterior and posterior imaging. For the first time, eyecare providers will be able to clearly visualize the cornea, vitreous, retina and posterior sclera in a single three-dimensional image, further revolutionizing clinical practices. As OCT technology continues to evolve, it will advance our understanding of eye disease and strengthen our ability to provide care.