 By Netan Choudhry, M.D, FRCSC and Jennifer George
By Netan Choudhry, M.D, FRCSC and Jennifer George
As people age, the gel that fills the centre of their eyes, known as the vitreous, liquefies and loses shape. This change in the vitreous results in its separation from the macula, which is located in the back of the eye. The separation, called posterior vitreous detachment, or PVD, is a normal part of aging. Sometimes, however, separation of the vitreous is incomplete, with small portions of the vitreous remaining attached to the retina. If this attachment leads to the pulling of the retina, the resulting condition is known as symptomatic vitreomacular adhesion (symptomatic VMA), which can lead to the distortion of a person’s vision, decreased vision and, in advanced cases, loss of central vision.
The retina is a thin layer of tissue making up the anterior lining of the inside of the eye. Located near the optic nerve, it receives light focused from the lens, which it then converts into neural signals to send to the brain. The macula, located in the centre of the retina, is the retina’s most sensitive region and is responsible for detailed central vision. Similar to posterior vitreous detachment, symptomatic VMA ordinarily occurs in individuals over the age of 50 and is most commonly seen in people over 70. It is also slightly more common in women and nearsighted individuals. However, the condition can occur in anyone, which makes regular appointments with an eyecare provider essential to catching symptomatic VMA in its early stage.
In individuals with symptomatic VMA, the shrinking vitreous gel moves away from the retina but remains partially attached. If the attached portions of the vitreous pull on the retina, it causes the appearance of flashing lights, stars or lightning streaks called flashes. Though the vitreous gel usually moves away from the retina without any problem, it sometimes pulls hard enough on the retina to cause a tear in one or more places. Fluid can then leak through the retinal tear, in which case the retina will lift off the back of the eye like a sticker peeling off paper. This is a serious condition known as retinal detachment.
Eyecare providers are now able to detect symptomatic VMA by performing a complete dilated eye examination and an optical coherence tomography (OCT) examination. The OCT will provide images of the vitreous and the retina, allowing for the accurate diagnosis of symptomatic vitreomacular adhesion.
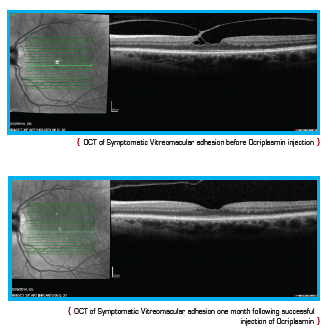 Current treatment options for symptomatic VMA include a period of watchful waiting, surgical removal of the vitreous gel known as vitrectomy, and the intraocular injection of medication. During vitrectomy, an ophthalmologist uses a small, combined cutting/suction tool in order to remove part of the vitreous gel, thus relieving the adhesion between the vitreous and retina. The removed vitreous gel is then replaced with fluid or a temporary gas bubble. Vitrectomy is only performed when patients are at risk of severe visual impairment or loss of central vision.
Current treatment options for symptomatic VMA include a period of watchful waiting, surgical removal of the vitreous gel known as vitrectomy, and the intraocular injection of medication. During vitrectomy, an ophthalmologist uses a small, combined cutting/suction tool in order to remove part of the vitreous gel, thus relieving the adhesion between the vitreous and retina. The removed vitreous gel is then replaced with fluid or a temporary gas bubble. Vitrectomy is only performed when patients are at risk of severe visual impairment or loss of central vision.
In recent years, a great deal of progress has been made in the treatment of age-related eye conditions but the key is still early detection. Regular visits to an eyecare provider remain essential to the prevention of severe cases of symptomatic VMA, macular holes and retinal detachment.