by Karin DuBois
 Lindsay Lenny remembers squinting through a cloudy haze as she drove her silver Volkswagen around Calgary. The 36-year-old administrative assistant had developed cataracts, a disabling eye condition commonly found in people twice her age. But unlike the majority of cataract sufferers, hers formed because of radiation treatments she had received for her leukemia.
Lindsay Lenny remembers squinting through a cloudy haze as she drove her silver Volkswagen around Calgary. The 36-year-old administrative assistant had developed cataracts, a disabling eye condition commonly found in people twice her age. But unlike the majority of cataract sufferers, hers formed because of radiation treatments she had received for her leukemia.
Lenny is part of a group of cancer survivors that develops cataracts as a side effect of radiation therapy. These cataracts affect a different part of the lens and are often more disabling than the common age-related kinds.
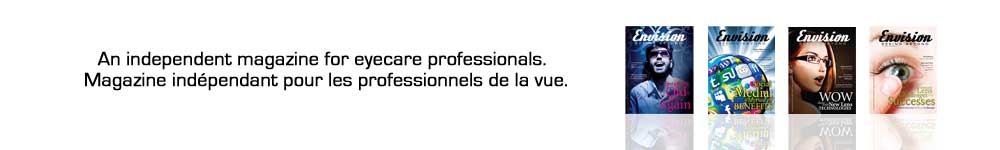
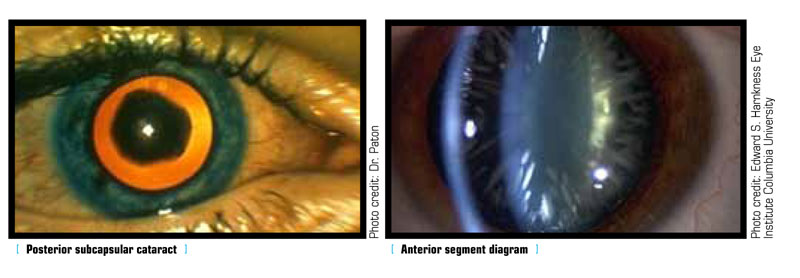
When radiation is used in cancer treatment, the goal is to destroy abnormal cells, but often innocent tissue nearby can be killed as well. If radiation goes through the lens of the eye, the cells in the equator of the lens – the area at the edge of the lens – can get damaged and lose their ability to divide. That’s when a cloudy cataract, usually a posterior subcapsular type, starts forming. Whether a cataract develops after radiation treatment to the eye depends on whether the lens was targeted, the dose and method of radiation and the patient’s general health.
“Often times when people are getting radiation, the trick is in the planning,” says Dr. Katherine Paton, an ocular oncologist at theUniversityofBritish Columbia. “If the tumour was behind the eye and you could come at it from the side without getting locked by bones you might try coming at it in a way to avoid the lens, but it might be in a location that your only option is to go straight through the lens.”
Dr. Paton says both the total dose of radiation to the lens and the dose per fraction – the amount given during each radiation treatment – can affect the likelihood of developing a cataract. In her experience, a radiation dose of 40 centigrade through the lens is more likely to produce a cataract than a patient who receives a lower dose. She says that steroids like Decadron also add to the risk.
“Even steroid medicine either given as an eye drop or as an inhaler for asthma or chronic sinusitis can contribute to cataract formation,” Dr. Paton says.
She adds that host factors – such as age and health – are also important. A diabetic elderly patient, for example, is at greater risk for cataracts than a young and otherwise healthy person, even when both patients have received the same radiation doses.
Radiation-induced cataracts can form as soon as 18 months to two years after treatment and often cause more glare and blur than the more common age-related types. Lenny, who had total body irradiation to treat her leukemia, began noticing light sensitivity and cloudy vision three years after her cancer treatment ended.
“Driving was the worst. There was a lot of glare and everything looked blurry,” Lenny remembers. She could no longer see the letters in road signs and started using landmarks to figure out where she was.
Dr. Paton says that Lenny’s experience is not uncommon, because unlike nuclear sclerosis, one of the age-related cataracts that can cause colour changes, people with posterior subcapsulars often see their surroundings as if they are obscured by an opaque bathroom window. The third type – called a cortical cataract – is commonly found in the elderly and causes distortion that is similar to looking through a glass bubble.
Radiation-induced cataracts are also physiologically different from the two age-related kinds. According to Dr. Paton, posterior subcapsulars are located deeper in the lens and closer to the center focusing point, resulting in more visual impairment than the other two types – which is exactly what Lenny experienced.
“It was like I was an old lady,” Lenny says, referring to how she felt when trying to read. “I would hold things up right up close to my nose and would be able to read them but I couldn’t read anything far away,” she says.
During cataract surgery, there is often scarring to deal with in posterior subcapsular types, a complication that is rare in age-related cataracts. According to Dr. Paton, the scarring looks like a plaque of dense material, and sometimes a laser procedure called an Yttrium aluminium garnet, or YAG, capsulotomy is required after surgery to completely remove the scarred tissue.
“The good news story is that cataracts are surgically treatable with really great results these days,” Dr. Paton says. She adds that even those requiring laser treatments after surgery can expect to have excellent visual results.
Today, after cataract surgery in both eyes, Lenny only needs reading glasses; otherwise, her vision is excellent.
“I wouldn’t hesitate now to go through it,” she says of her cataract surgery. “It will change your life back to normal where you can actually see and you don’t have to worry about your eyes ever again.”